I have had a couple of touchy discussions with patients last week about addressing all of the issues contributing to their chronic pain and inflammation status. As with most touchy discussions, they revolve around lifestyle issues that patients are often struggling to change or prefer to be in denial about.
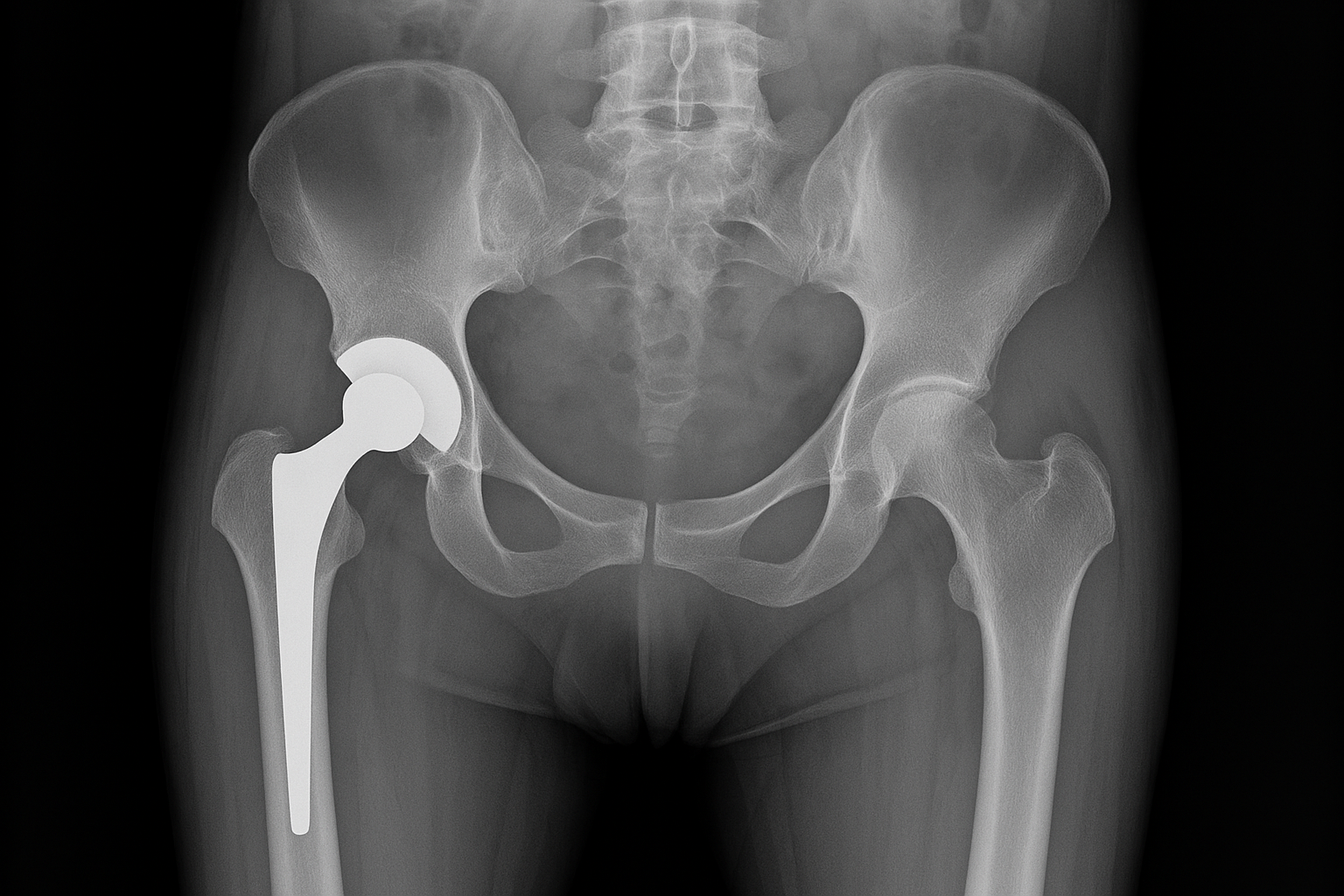
One of those discussions revolved around the role of excess weight. The stats are telling us that our collective BMIs are going up, and I certainly can attest to that in the microcosm of our office. Patient can begrudgingly understand the mechanical impact of excess weight on a downstream joint complex. What is overlooked in the process is the contribution of excess adipose tissue (stored excess fat), in powerfully adding to the pro-inflammatory chemical soup of our bodies. Body fat is far from being an inert blob hanging on to your belly or thighs. In reality, it is a very active endocrine and metabolic tissue that secretes a variety of chemicals. One of those chemicals is called “adipokines”. These substances modulate inflammation control. When body fat is unregulated due to increased storage, the secretion of “pro-inflammatory” substances is elevated and pretty much never goes down until the body fat levels starts to return to a body fat percentage that is more normal. So in individuals with elevated BMIs (AKA overweight or obese), there is an increased likelihood of chronic inflammation affecting joints, ligaments, cartilage, brain, heart, and that compounds the mechanical effect of the excess weight. For those individuals, shifting to a more anti-inflammatory diet pattern, while you slowly work out your weight issues, and possibly adding some anti-inflammatory supplementation to your regimen, may be necessary to mitigate chronic pain.