That was the literal question posed by a patient last week, who had realized that just about everyone else in her circle of friends and family had received the same diagnosis. It was a fair question and here is how I would respond:
Design: The cervical spine is designed with maximum flexibility in mind for humans to be able to respond quickly to their environment, looking up, down, and to the sides rapidly and with ease. The cost of flexibility is susceptibility to trauma, and beyond a certain threshold, the cervical disc cannot recover and deteriorates.
Repetitive Postural Trauma: The cervical spine has a normal forward curve that gives it a certain amount of stability to forces like jarring, brisk side to side movement, and compression from above. The modern lifestyle does a lot to disrupt the normal forward curve by forcing it into a straight or reversed position: everything is in front of us and below eye level. The recent addition of small devices like tablets and smartphones have us looking downward for prolonged periods of time more than at any other time in human history.
Acute Trauma: Modern life has added high speed collisions as a potential trauma for which the cervical spine is completely unequipped. Prior to the 19th century, the highest acceleration injury to your cervical spine is likely happening when you trip and your head hits the ground, arguably a pretty hefty force. But vehicles travel at a speed of 70 MPH or higher, and the combination of a 70 MPH sudden deceleration times the mass effect of a vehicle is the type of force that our delicate cervical spine is not meant to handle. Over a lifetime, just about any person living in an industrialized country will have to contend with one good whiplash. And those types of injuries, often sustained during our early driving years, can set a pattern of early degeneration that will stick with you for a lifetime.
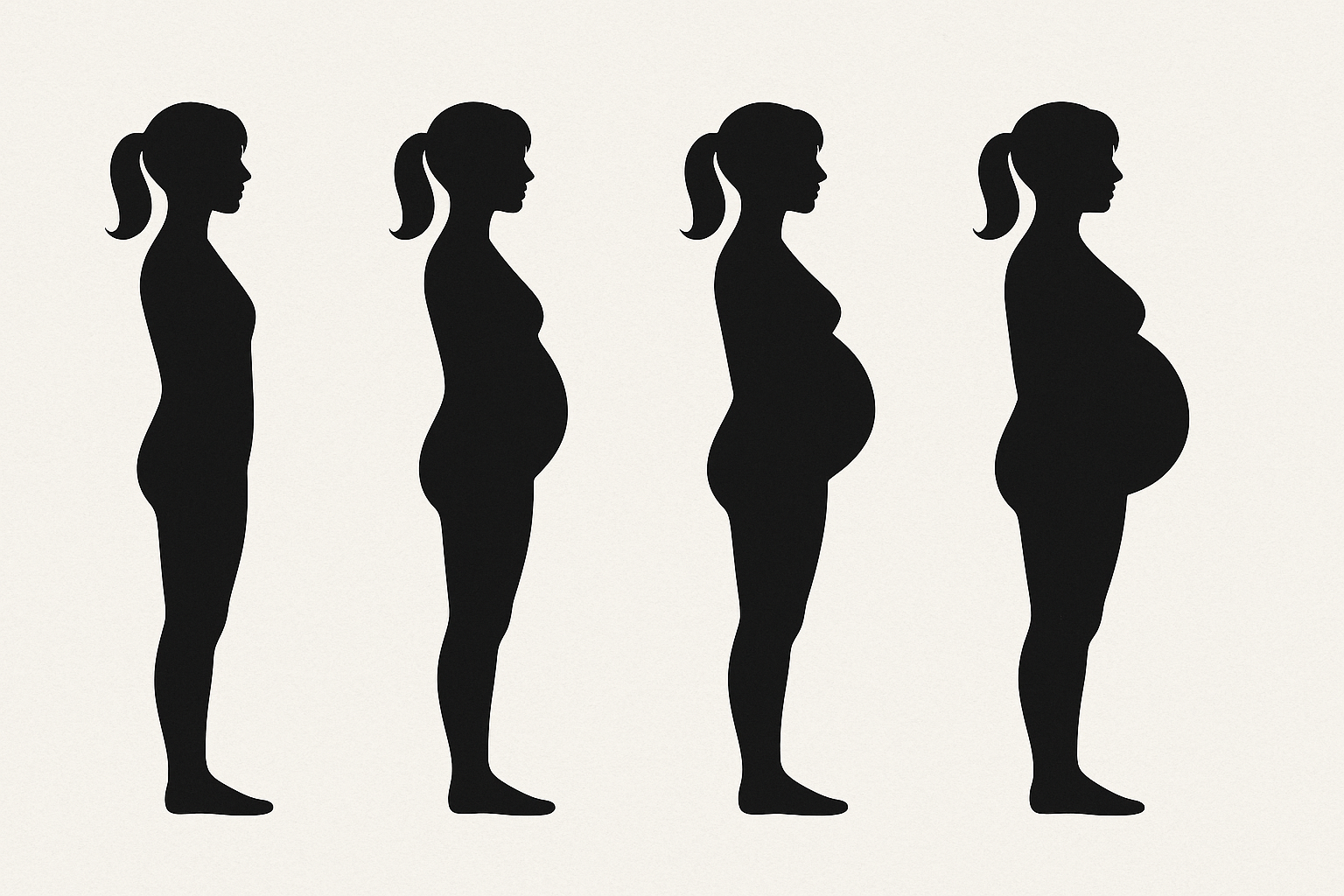
Metabolic Changes Affecting the Longevity of the Spinal Disc: Probably a highly overlooked factor. The “chemical soup” of our body chemistry is the matrix bathing our spinal discs and facets joints, and that matrix needs to provide the repair nutrients and waste removal system to repair daily microtraumas as well as larger single traumas. The combination of the average highly inflammatory modern diets, low essential nutrients, environmental toxins, and low oxygen conditions of deconditioning are the perfect storm that compounds the other factors and limits the body’s ability to recover and repair.