There are two important health issues that are on the apparent periphery of what I do on a daily basis, but their impact on people's long-term health, as well as indirectly on the quality of the recovery we can achieve through our care, is important enough that I often feel the need to bring it up. I did previously blog about one of them, uncorrected acquired hearing loss, and today I want to briefly touch base on the other one, which is obstructive sleep apnea.
For our purposes I would define sleep apnea as the inability to maintain proper respiration during sleep, resulting in insufficient oxygen delivery to all tissues in the body but the central nervous system in particular. Loud snoring or choking associated with the obstructive version of sleep apnea can further disrupt people sleep by continuously waking up the patient.
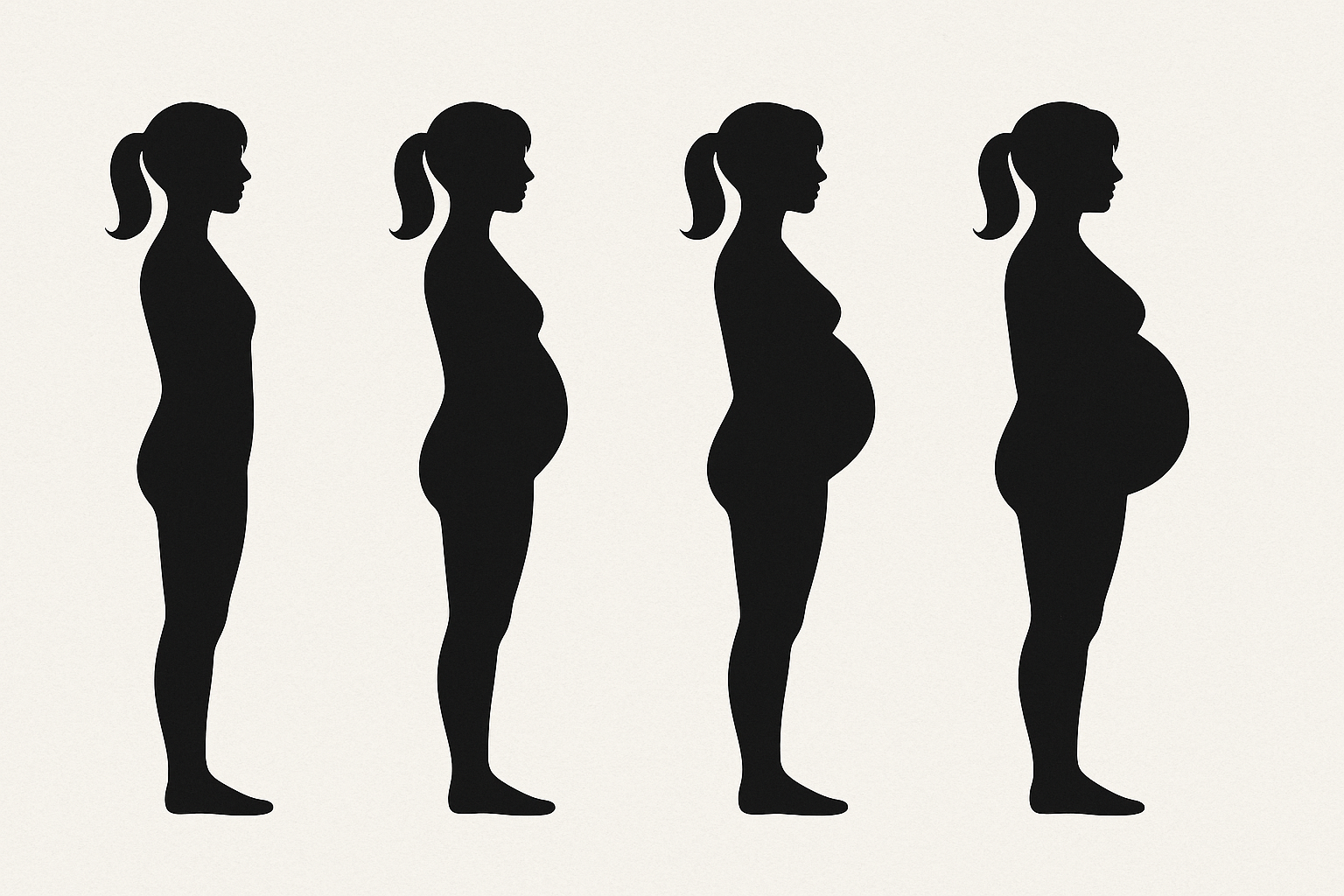
Ignorance in this instance, is clearly not bliss. The current treatment of sleep apnea is still somewhat rudimentary, mostly using CPAP machines which not everyone feels comfortable using, (with a few emerging alternative options for some patients such as oral appliances), leaving most people to go in denial mode and refusing to be screened and diagnosed. I often have suspicions of sleep apnea based on patient's symptoms, cognitive changes, body shape and BMI, neck and head morphology. I will ask questions, and strongly recommend screening. Some people prefer to brush me off or let my suggestions fall on deaf ears. In this article I have attached a link to a particularly sobering research article which highlights why it's a very poor strategy. Sleep apnea is not just a mild annoyance, it has severe ramifications on premature aging and mortality. By the time the patient may decide to heed the recommendation, the damage may already be done and reversible. Literally down to the level of damaging your genes.
One legitimate concern brought up by some people is how to access meaning and diagnosis. A full-fledged sleep lab testing runs in the thousands of dollars, often a financial strain on patients with high deductible and coinsurances. In some instances when patients have adequate insurance coverage, they do not meet the insurance set criteria to be eligible for the test into first place.
While not exactly an exact replacement, the availability of over-the-counter home sleep apnea screening kits can still fill the gap with pretty dependable screening measurements of heart rate, breathing rate, and oxygen saturation overnight in the comfort of your own home and your own bed.
https://erj.ersjournals.com/content/59/4/2103042
https://www.google.com/shopping/product/1?q=watchPAT+home+test&prds=epd:17928710654120051378,eto:17928710654120051378_0,pid:17928710654120051378&sa=X&ved=0ahUKEwibhsGTzef4AhW7rIkEHZoaACoQ9pwGCAU