This is another overdue blog series, long overdue actually. I keep telling patients with whom we have discussions about chronic soft tissue problems throughout their bodies that I'm going to put the summary of our recommendations in writing in an easy patient reference on our website. But it's a bit of a bigger brainchild than some of my other blogs and has required a bigger bandwidth of time than I've had for a while.
This series is designed to address some key concepts about what is basic necessity to keep your soft tissues healthy, and self repairing. By soft tissues and I mean anything that's not a bony tissue, ligaments, tendons, muscles, fascia .The key nutrients that maintain soft tissue health and self repair are often a little different than what our patients understand, leading them to invest a lot of time resource and energy in the wrong solutions.
Soft tissue problems can be manifested in any part of your neuromusculoskeletal system, and can be very local and regional, related to injury, or widespread, which may have more of a metabolic component. They affect the spine and the limbs. This series of informational blogs would be especially geared towards people who have either widespread soft tissue pain and susceptibility to injury with poor repair, as well as patients who had one major soft tissue injury and do not seem to be able to recover on schedule.
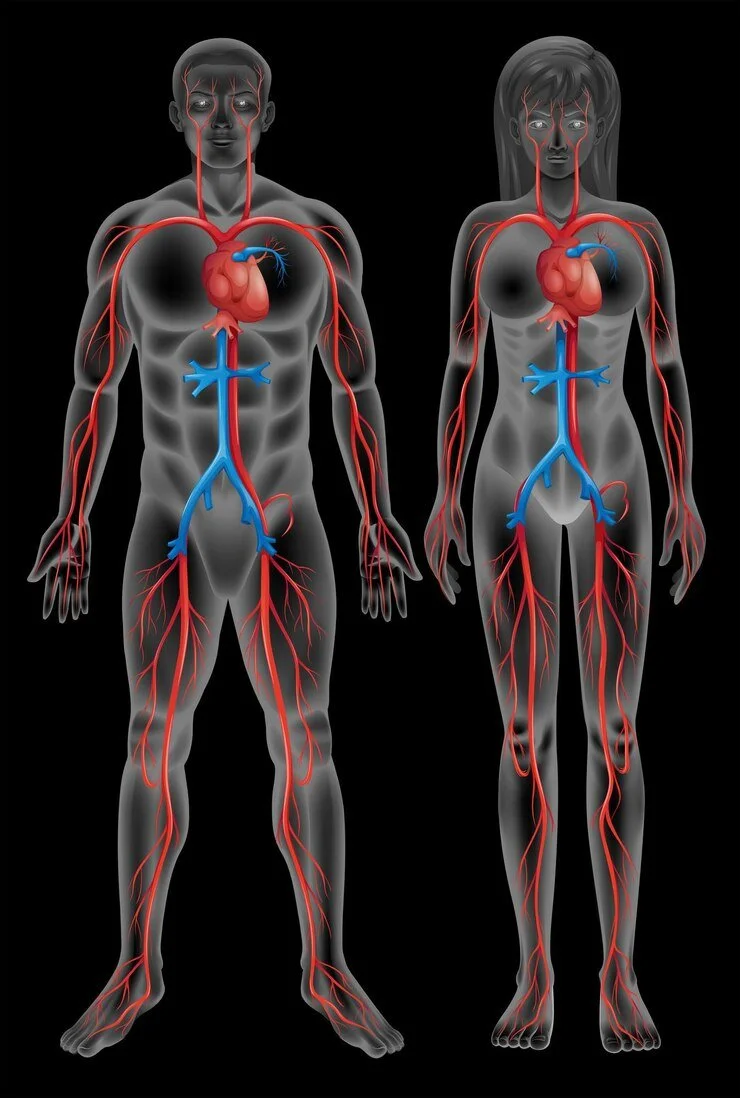
The 1st nutrient we need to talk about in regards to soft tissue health is blood flow. Without adequate circulation to soft tissues, key nutrients that will be described in later blogs, such as oxygen, glucose, electrolytes cannot be delivered to the tissue. Blood flow is of clinical relevance because the mechanism of blood delivery to soft tissues can be easily impaired by trauma, both single acute trauma as well as repetitive sub traumatic forces.
Blood flow to tissues can be suboptimal under many circumstances, some of them general and metabolic and some of them more local:
– cardiovascular issues with low cardiac output, general cardiovascular deconditioning (the latter is more prevalent than people realize), medications that slow down the heart rate
– peripheral vascular disease that narrows blood vessels, especially small blood vessels called capillaries ( think diabetes and pre-diabetes)
– autonomic dysfunction affecting normal dilation of blood vessels under increased demand such as physical activity
– peripheral vascular disease such as obstructed blood vessels from atherosclerosis or calcification, especially if it affects large arteries going into the limb, for example the femoral artery
– smoking. It has a huge impact on the health of blood vessels, making them less flexible, and more easily permanently contracted under the effect of nicotine, decreasing peripheral blood flow.
– Scar tissue in the muscle from previous injuries. I find that to be the most common issue outside of the above general health and metabolic issues. Injuries, both single traumatic injuries and repetitive micro trauma such as repetitive strain injuries, can result in replacement of normal flexible connective tissue with much harder shorter and less flexible collagen, which prevents the normal extension of fine blood vessels and decreases the amount of blood flow perfusing through peripheral tissues. This cycle of decreased blood flow from scar tissue is further aggravated under certain circumstances including cold exposure, and varying degrees of additional muscle spasm, or certain compression garments.
Addressing blood flow issues for soft tissue health will obviously depends upon the nature of the blood flow interruption. In some cases, it's more easily achieved than others, as the case of some cardiovascular conditions and medications that are nonmodifiable, and will require some adjustments of soft tissue recovery expectation as a result.
Photo courtesy of Freepik
–