An increasing percentage of our population is living above 65, and often for another 2 or 3 decades. This bit of good news if you're approaching that milestone (I am!), Is that you have 2 or 3 more decades to experience and hopefully enjoy life. The bit of bad news is that you will get to live out those 3 decades in a body facing increasing wear and tear.
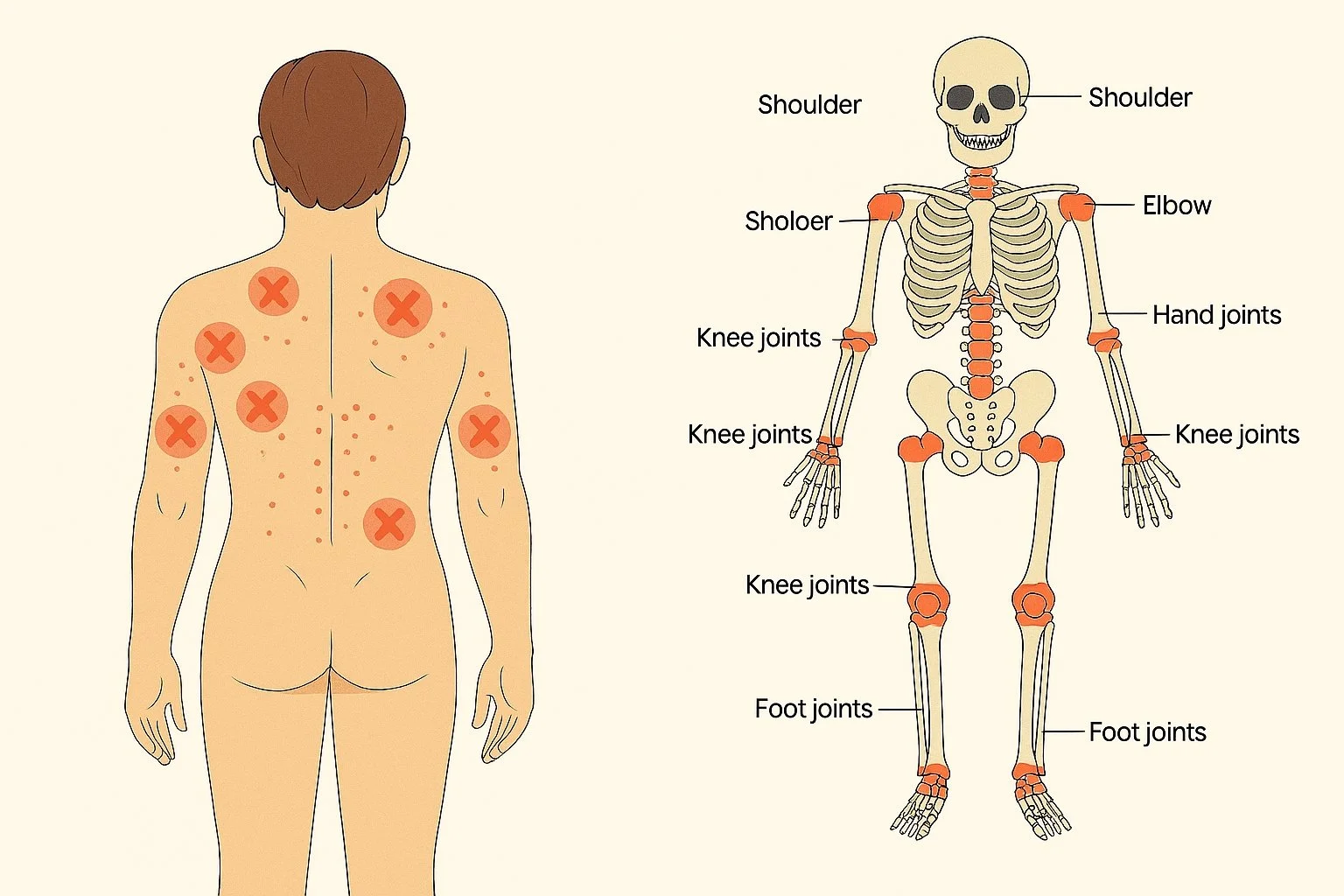
Osteoarthritis refers to the process by which articular cartilage starts to deteriorate, leading to loss of joint space, and a constellation of associated structural findings and symptoms: instability, spurring, loss of normal motion, chronic pain and inflammation. It should be noted that osteoarthritis is not a linear finding correlating with simply aging. Some patients are more predisposed to osteoarthritis than others because of additional mechanical factors causing accelerated wear and tear on joints of the spine and extremities (which is why chiropractic research has shown some modulation of progressive osteoarthritis in many patient receiving care, reducing unnecessary mechanical stress). Other patients experience worse osteoarthritis because of metabolic factors that have to do with our poor nutrition, lack of blood flow from inadequate physical activity, and other complications from health issues such as medications, medical treatments etc.
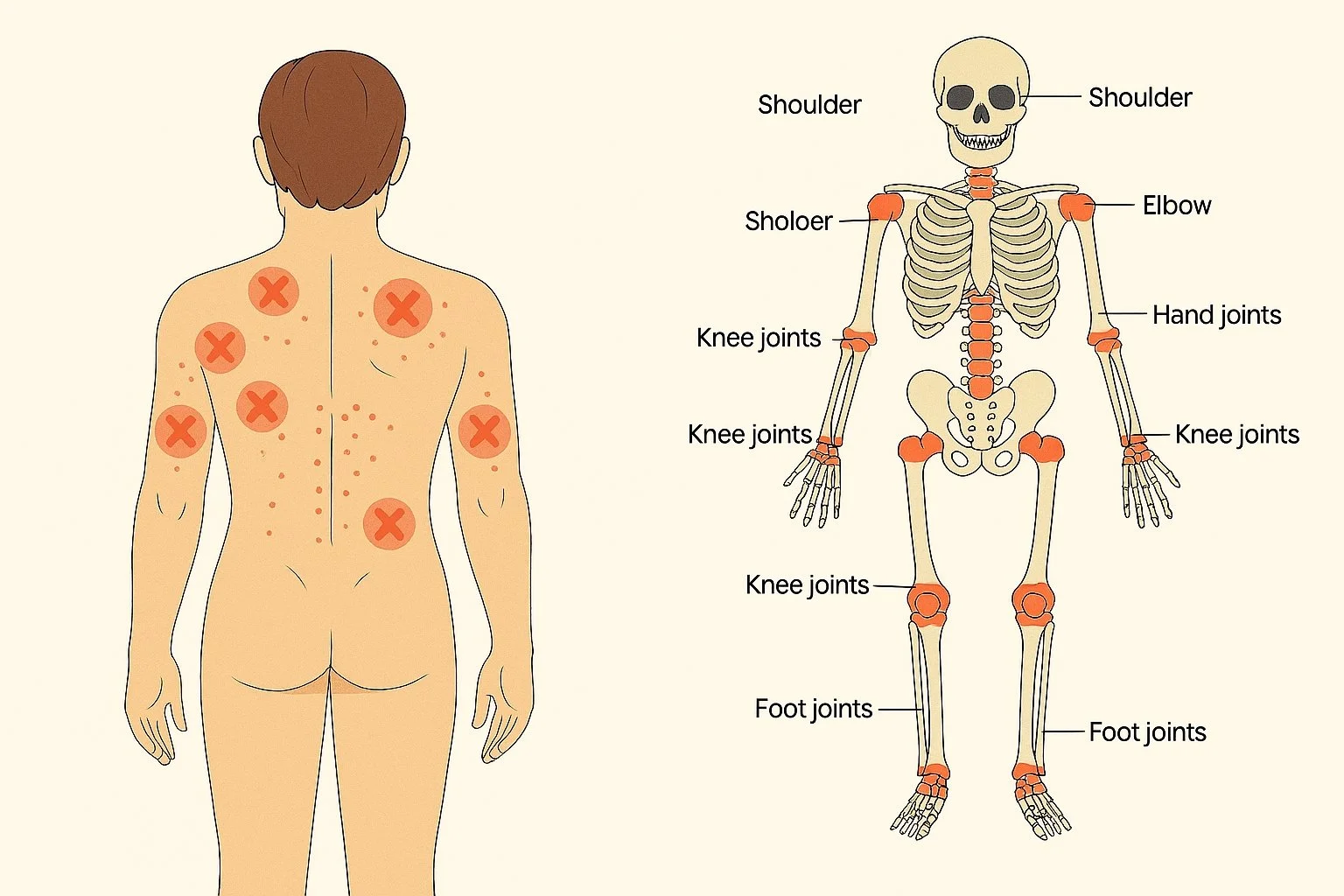
One aspect of the constellation of osteoarthritis related findings and symptoms that is often missed or poorly understood is the secondary chronic myofascial pain syndrome and widespread trigger points. There are complex reasons for that that have to do with the local neurology of the deteriorating joint on muscular tone and control. Patients often are frustrated about what they believe to be a completely new problem, until we sit down and explain to them the correlation between myofascial pain syndrome and osteoarthritis, as being the manifestations of one common phenomenon. But there is something unnerving about patients suddenly feeling that every muscle tendon and ligament in their body is starting to hurt.
Myofascial pain syndrome and trigger pointsin the context of osteoarthritis should be treated both concurrently for the best results. Addressing the myofascial pain alone will have little to no lasting results since there's an upstream trigger. Joint adjustments, active range of motion exercise and strengthening, information control will hugely impact the severity of the myofascial pain. Conversely, only addressing the osteoarthritis will often fail to adequately resolve the myofascial pain since it often has become a self-perpetuating condition of its own.
Myofascial interventions in patients with moderate to severe osteoarthritis does need some modifications. Levels of pressure, frequency of treatment need to be adjusted down. Qualified soft tissue therapist know how to modify the treatment plan accordingly. Other supporting treatments that have found to be very effective are dry needling, traditional acupuncture needling with caution, as well as a variety of topical intervention such as infrared therapy and counter irritant topicals
https://pubmed.ncbi.nlm.nih.gov/36943163/