I recall running into one of the first editions of this book during my last year of chiropractic training ( 29 years ago…) The resource library of the school satellite clinic had that among the many great patient resources that could be checked out, along with books on stretching and the first anti-inflammatory diet. Among us intern students, it was certainly a more popular read than some of the useful, dry material of the other books, and the fodder for much chuckle and smart talk. Most of us were still in our 20s, still a wee bit green in our real world clinical experience, and certainly able to athletically engage in our amorous pursuits ourselves - in other words, very ill equipped to field questions much less give useful answers to the patients who were not.
I recall frantically looking for “the Book” after my second month in practice in Cannon Falls. A lovely 80 year old gentleman limped his way into the office that week with a very nasty, hot sacroiliac sprain. Which, he candidly described, went out on him while he was “ being conjugal” (sic) with his wife of 57 years. His problem responded to care quickly, but just as quickly came the question of what he shouldn’t do and how he should not do it in order to avoid a reinjury, as his lady was apparently quite eager to pick up where they left off. In spite of my liberal European upbringing, I felt a bit under-resourced to properly advise him on the subject.
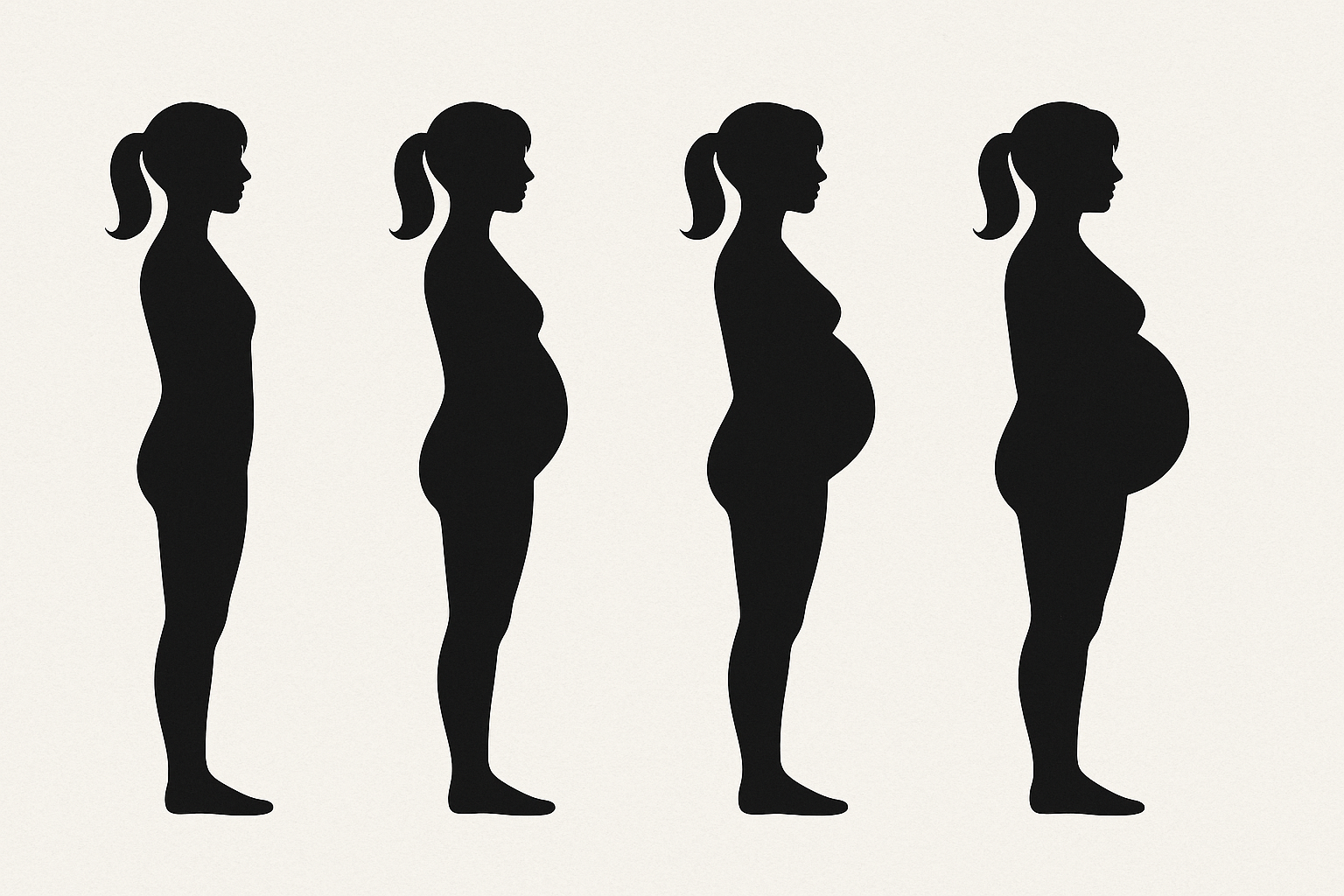
Sexual activity is no different than doing your job, your sports, cleaning your house, and doing your favorite hobby: if you have a significant spinal injury, or a more chronic degenerative issue, you have to know how to make some modifications to make it happen safely and comfortably, so that you continue to do what is important in your life rather than give up on it all together. This is not an uncommon subject that we have to broach in the office, and beyond the basics, I have found this book to be still very relevant and informative.
https://www.amazon.com/Sex-Back-Pain-Restoring-Comfortable/dp/1879864029/ref=sr_1_3?crid=3DXFL4XVDFNCJ&keywords=book+sex+and+back+pain&qid=1645760200&sprefix=book+sex+and+back+pain%2Caps%2C126&sr=8-3