Several of our patients are opting in for planned joint replacements of hips and knees at this season, with the assumption that their work on their rehab and be ready to hit the ground for the season of outdoor gardening vacationing and general fun summer activities with some new and well-functioning hardware. This reminded me of a long-awaited blog as I've seen several cases last year.
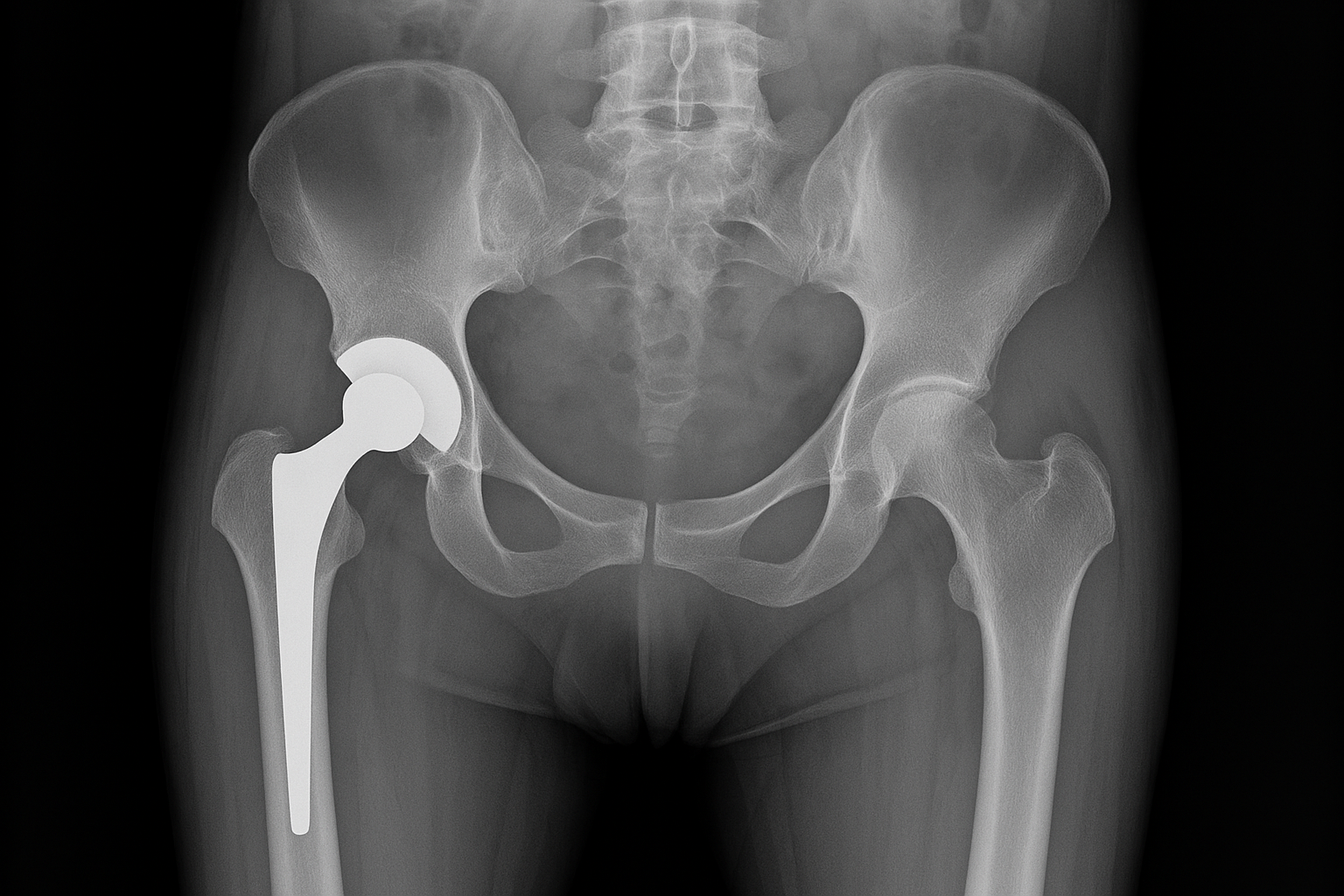
I've been in practice 32 years and 1 of the most stunning improvement I've seen that affect my patients in my practice has clearly been the advancement in joint replacement. Minimally invasive, robotics, short recovery, they sometimes come with some challenges that need to be addressed so that the patient has the optimal recovery they're looking for by going under the knife. One such challenge is sudden changes in leg differential that can happen even when surgical intervention has been optimal.
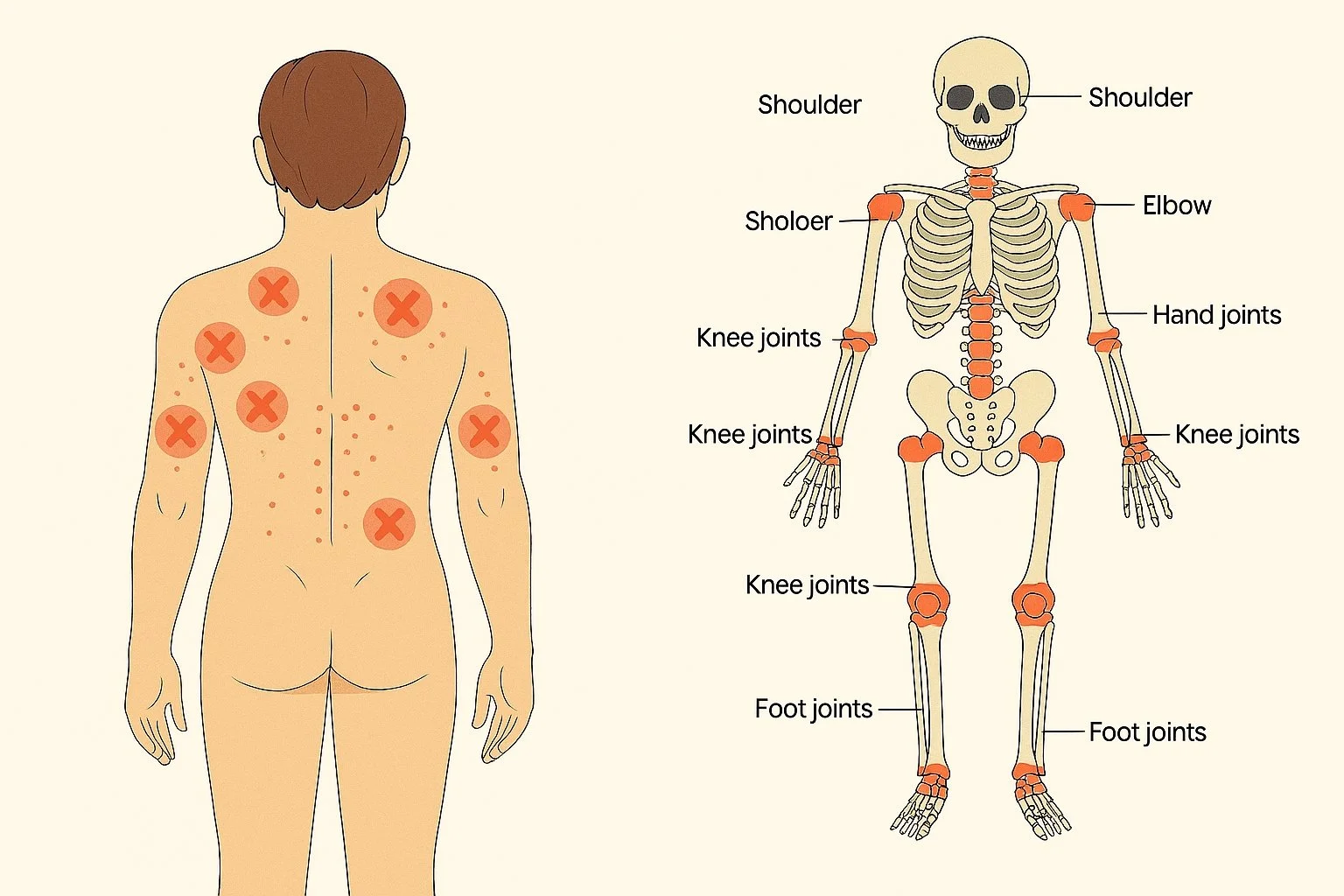
The process of osteoarthritis and articular cartilage joint loss is a slow process that happens over years. The thickness of an intact joint versus that of a fully deteriorated joint can be over 1/2 an inch in difference. (Maybe closer to three quarters of an inch at the knee because of the presence of the meniscus). As a result, the leg affected could be easily an inch shorter from its original status, a process that the body will be able to mostly absorb over time due to its ability to slowly compensate at several levels including the sacroiliac, the lumbar spine, and the ankle.
A joint replacement will overnight reestablish the distance of a joint to its original state, and that can paradoxically be a real big problem. While the body can adjust to half an inch of difference in leg differential that gradually manifests over 2 decades, it doesn't have the ability to adapt to three quarters of an inch overnight. As a side note I should mention that our fine orthopedic surgeons have done an increasingly better job at trying to assess the leg differential and compensate for that during the surgery. But it's not always a perfect process and some surgeries come with inherently more difficulty in maintaining equal leg length, especially for people who have profound damage to the bone in which the prosthesis is going to be inserted (previous fracture of the limb, AVN, osteonecrosis, hip dysplasia, aggressive subchondral cysts to name a few).
The typical presentation looks like this: patient has successful surgery, discharge into rehab. Within a few days of starting to ambulate, they start developing intense pain on one side of their lower back and gluteal area, often the opposite side of the hip or knee replacement. Initially they write it off to limping prior to the surgery or after to the surgery, but the pain only deteriorates as they increase their walking time.
Sometimes the process goes on for a few years before I happen to see the patient. The history will reveal a pretty clear correlation between the surgery and are rather rapid onset of the new pain pattern post surgically and related to increase weight bearing time. During the patient's physical examination, when I observed them standing from the front to the back and walking, is a clear pattern of a very tilted pelvis, most often high on the prosthetic side. By the time the patient has been ambulating with an acutely acquired noncompensated long leg, did create some mechanical stress that will require some manual intervention with chiropractic adjustments, soft tissue mobilization and sometimes some balancing exercises. But as soon as is feasible in the body can tolerate it, I'll start inserting a heel or full-length foot lift gradually, to bring the pelvis and the lumbar spine to its original level. There is some real finesse and how you conduct the leg balancing, often having to start with a few millimeters at the time and increase by a couple millimeters every 2 weeks, and due to complications of mature hips and knees on the affected side, most often will require a full-length lift which sometimes will have to be external in the shoes. I should also note that we don't always have to compensate for the full deficit, but the body will often be able to adapt to approximately half of the leg differential and will just need to shim for the other half. However, the recovery by addressing the acquired long leg from a joint replacement can also be very dramatic and rapid, making everyone happy.
The moral of the story: if you are having some persistent new unilateral hip lower back or thigh pain after a lower extremity joint replacement, don't give up on yourself and be evaluated. It could be a relatively simple problem to resolve.