Whiplash as a public health epidemic: a hard look at real data to call it what it is.
https://pubmed.ncbi.nlm.nih.gov/32413544/https://pubmed.ncbi.nlm.nih.gov/32413544/
More recently I have been back on a nerd Safari listening to research podcasts. The most recent series focuses on the career research work of highlighted individuals who happen to have a chiropractic background but later expanded into other health disciplinary approaches. One of the most fascinating individuals in that series is Michael Freeman, third-generation chiropractor who spent the first 12 years of his worklife is a small town chiropractor on the West Coast, later to get a medical degree, public health degree, and multiple specialty additional degrees and certifications in forensics and epidemiology. His initial focus was to better understand the morbidity and mortality of crashes and accidents, especially motor vehicle accidents. I could certainly relate to his dilemma, facing the reality of these low-speed collision injuries in practice, while being told by the "official" date at that such injuries did not really exist.
The space of motor vehicle accident injuries is fraught with conflicting interest. There is certainly a lot of press given to the idea that patients are financially motivated when reporting persistent residuals from injuries, including injuries that happen at relatively low speed and with relatively little vehicle damage (which will be the topic of a subsequent blog). There is also the official statistics from national crash data reporting systems, suggesting that certain types of injuries such as cervical disc prolapses, happen extremely really at low speed collisions. Then again something that conflicts with my observation in 32 years of practice.
The other side of the story is that there is an equal if not higher level of financial motivation on behalf of the payers in the insurance industry. Profit depends upon paying out less in claims than you taken in premiums obviously. And to be fair, I I have seen my share of poor and questionable business practices in some of my colleagues over the last 32 years, who were willing to amplify the treatment needs of people in motor vehicle accidents because you could bill the car insurance company at a higher rate and for more visits than you could a commercial policy. And yet, overwhelmingly, I saw more people with real nasty persistent, difficult to treat and stabilize injuries, that had their benefits cut off long before they had reached the maximum recovery, by insurance claims adjuster hiding themselves behind certain statistics. Some of the statistics never made any sense to clinical providers like myself and my colleagues, and it has taken the hard work of people with strong data background and unquestionable research methodology to counter the narrative put forth by the insurance payers.
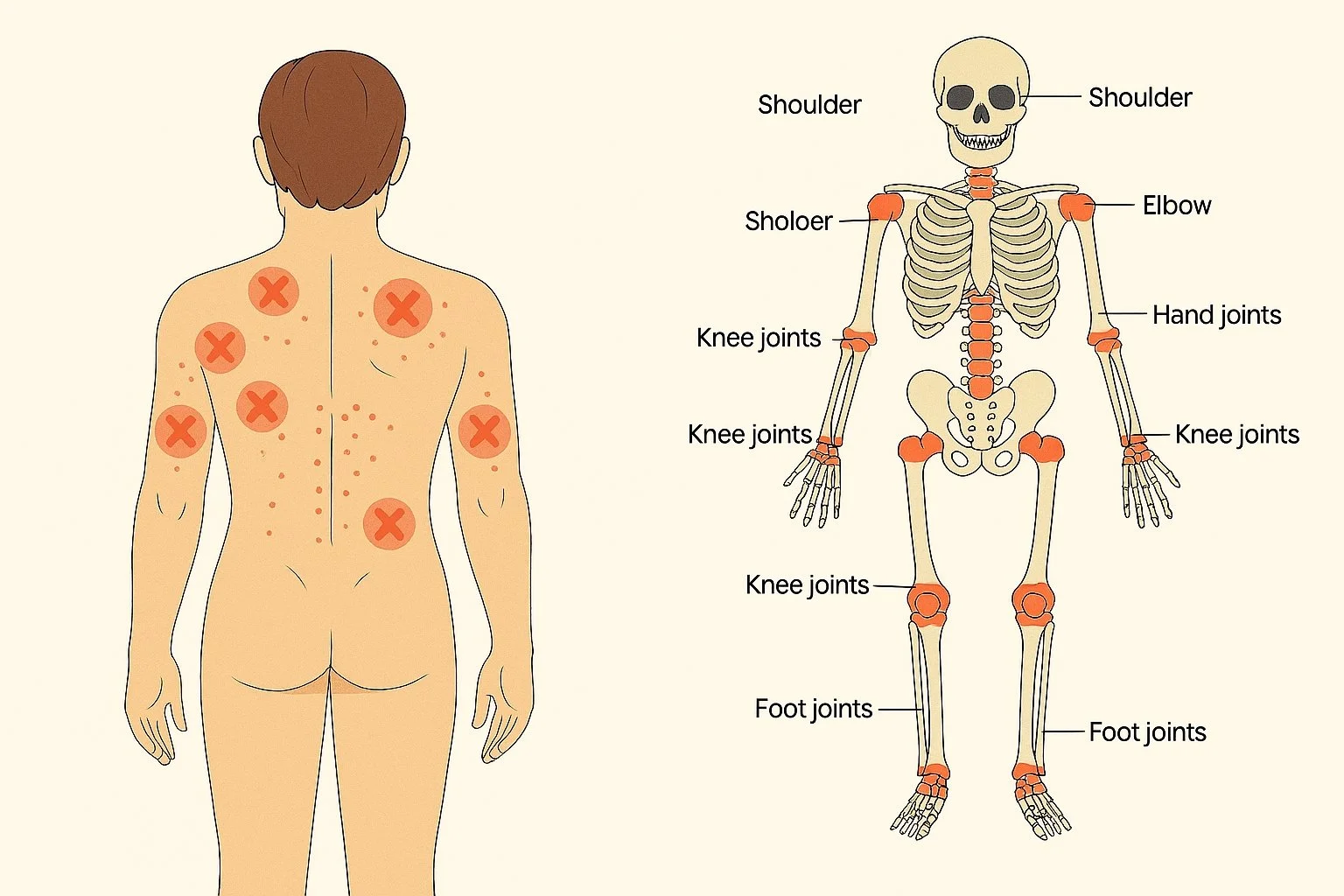
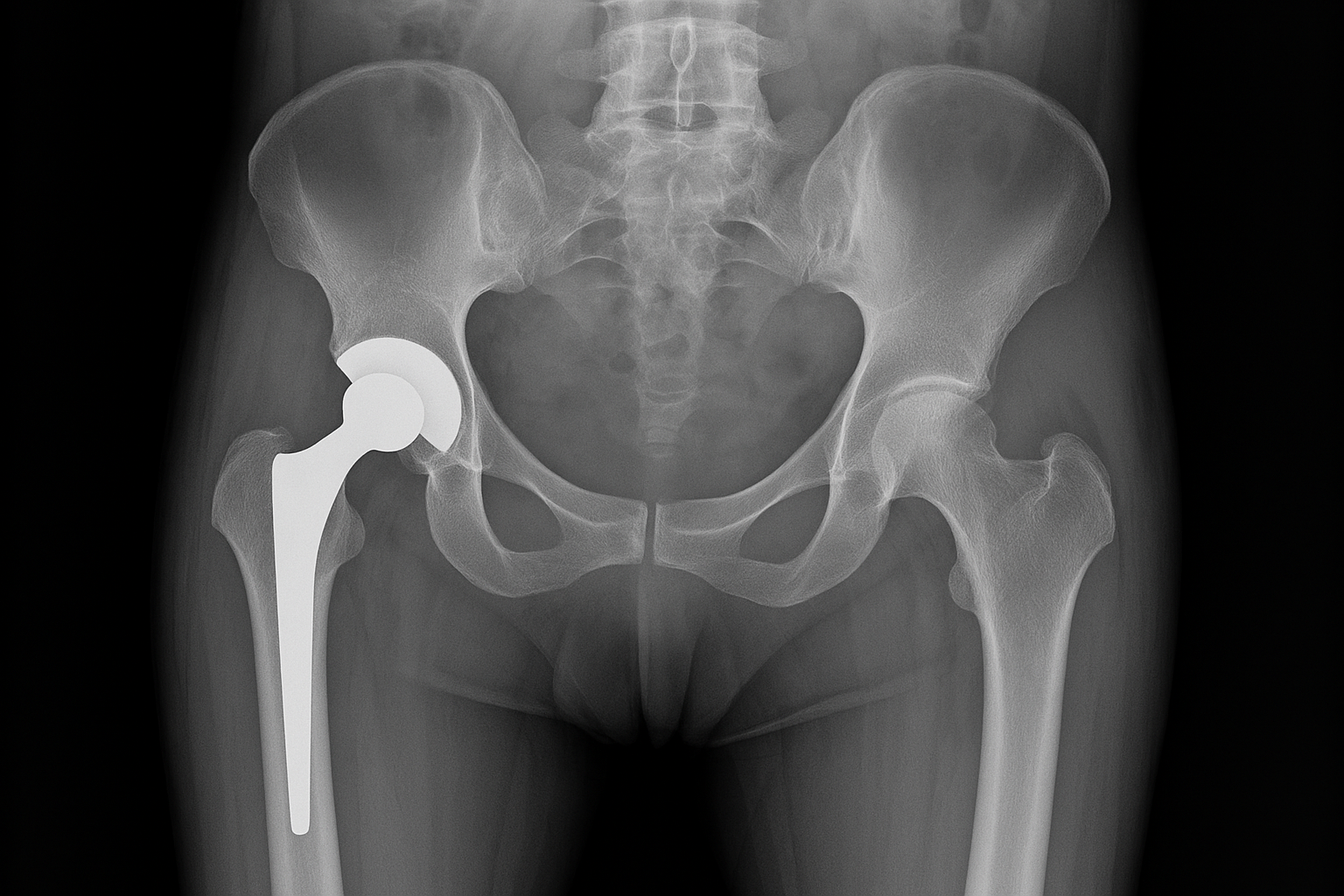
Enters Michael Freeman and his work. This particular study focuses on the actual incidence of cervical spine injuries from motor vehicle accidents in the US, using more accurate data from hospital reporting ER visits for motor vehicle injuries to the cervical spine. His research paper also highlights the extreme limitations of the crash reporting data reported by insurance companies, which only look at the first 48 hours of reported injuries following a motor vehicle accident. Unless you're dealing with a fracture, internal bleeding or severe head injury, the majority of people in low to medium speed collision haven't even made it to urgent care 48 hours after the crash: their adrenaline is so high and blocking pain they did not fully capture the level of the injuries, they are overwhelmed trying to figure out their damaged vehicle situation and get replacement wheels to get to work, they're trying to figure out what sort of injury coverage they may have before incurring a huge medical bill etc. Of most interest to me in the study was the discussion about cervical disc injuries. I see those remarkably frequently in collision speeds of 10 miles an hour or less, depending upon other factors associated with the crash such as speed of impact, position of the passenger etc. The official crash statistics tell you they almost never happen, however almost nobody in the low-speed crash will have a cervical MRI in the first 48 hours after an accident, which is the only way to truly diagnose those types of injuries. This is confirmed by Michael Freeman study, which shows that based on hospital statistics alone (and that's even an underestimate of cervical disc injuries since many of them will not have their MRI until they walk into our office three months later with persistent pain from the original accident), 92% of cervical disc injuries are missed by the official crash statistics.
I had the pleasure of listening to an interview by Dr. Freeman recently. In his own words, cervical injuries from motor vehicle accidents are so prevalent, estimated at 1.2 million injuries per year in the US, that we really should think of them as a public health epidemic, considering the morbidity and disability associated with the immediate injury, much less the potential percentage of people who will continue on with chronic persistent symptoms. This certainly resonates with me as a practitioner with a large practice in chronic care management, where people will often show up with a constellation of symptoms that they clearly date back to an original rear end collision 30 years prior.
The moral of the story: whether your patient or doctor, you need to sometimes block off the so-called official statistics, and really look at what your individual situation tells you. If you were in a crash, and within a couple weeks do not develop any symptoms, you're probably not injured. But if you're in an accident, and you start developing pain that is new or unusual for you, regardless of how little scratches you see on the bumper, you need to consider the possibility of an injury and not delay treatment.