july seems to be the time when of our teens tackle some ruthless sports training camp. I've seen a fair amount of those beat up bodies, full of new muscle bundles and a few injuries, show up for treatment at the office. This flood of athletic teens has reminded me of an important topic I've meant to blog about for a while.
Adolescence seems to be a time when migraine patterns can emerge. Hormones get a lot of the blame, and there is some partial truth to that, although I feel that it's often an easy copout without looking at other causes. (Much less trying to understand hormone imbalance and correct them). Injuries to the cervical thoracic spine, athletic head injuries, and some nutritional deficiencies can also be a huge trigger in genetically predisposed individuals. The good news is that there is some recovery path available. Today I want to talk about one particular subset that affects especially young athletic females. The pattern and distribution of the migraine is similar to other migraine headaches, but the timing seems to often coincide at the end of physical activity, indicating a metabolic trigger to the headaches, as at the end of the menstrual cycle rather than before or during menstruation. Over time however, the temporal correlation to exercise and menstruation becomes less clear as the migraine pattern becomes more frequent.
Migraines can have multiple triggers. One common mechanism among many migraine patients is the drop in available energy production in the central nervous system, since neurons hold a negative charge that requires a lot of continuous energy production in the brain in order to be maintained. If the energy production drops very suddenly, or persistently, the neurons lose their charge and can fire in large patterns, causing a random wave of what's called depolarization that can lead to a migraine.
Energy production in the brain requires several things: stable blood sugar (some people can metabolically adapt to ketone fats as an energy substitute for non-high-intensity activities), adequate blood flow, adequate oxygen concentration, adequate electrolytes balance. So episodes of hypoglycemia and low electrolytes can definitely be a ripe terrain for migraine to spike. I think most teenagers and their parents have already figure that out with pre-exercise electrolyte as well as making sure they've had some sort of preexercise snack.
The contribution of low oxygen concentration however does not seem to be on many people's radar. This happens mostly when a teenager is borderline anemic, or has low iron/low iron reserves. Oxygen concentration in the brain is dependent upon not only the blood flow to the brain but also the amount of oxygen carried by hemoglobin in the red blood cells.
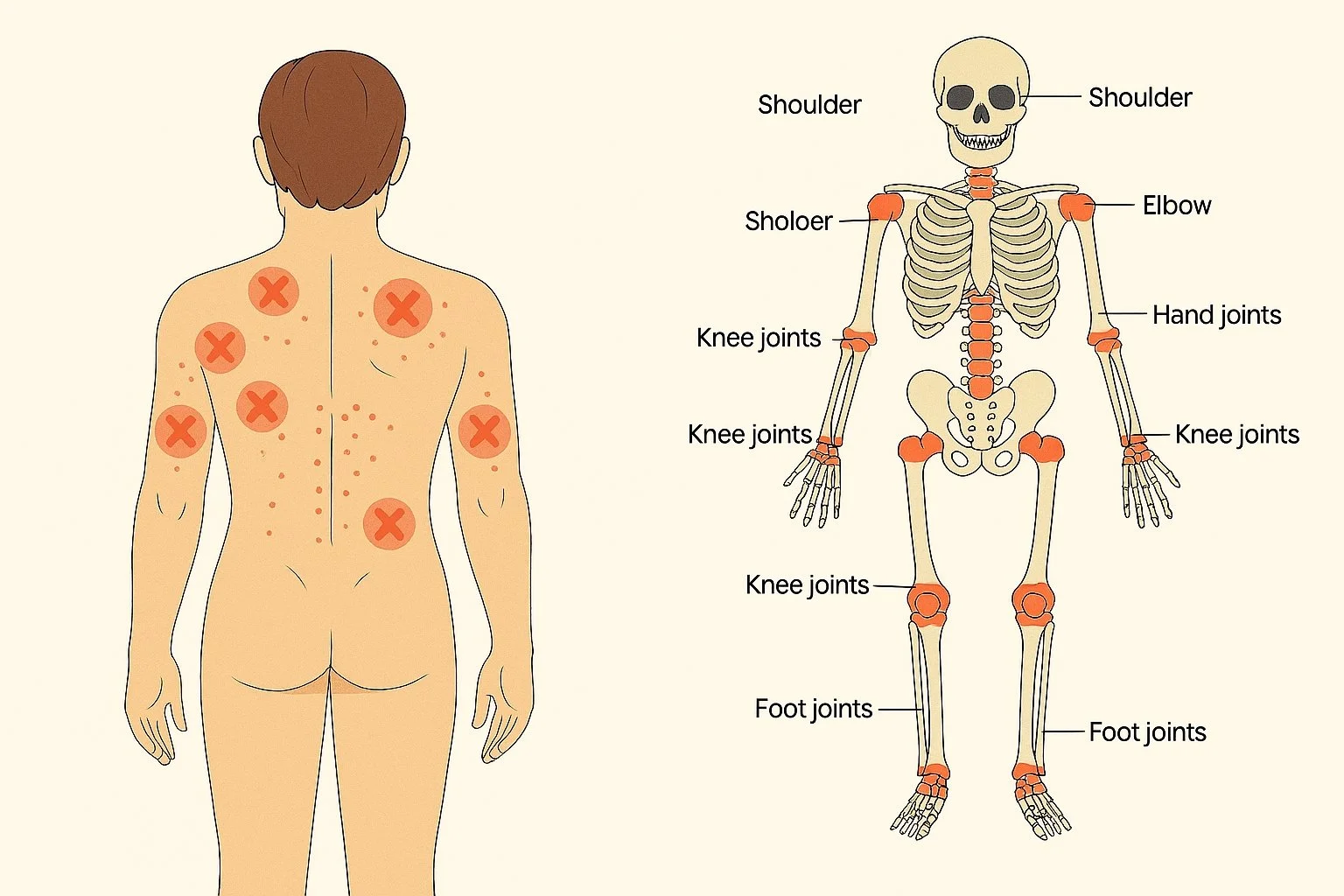
Young athletic females are especially vulnerable to iron deficiency anemia or low iron reserves because of three main factors:
– adolescent females menstruate, often at the time that they pick up the intensity of the athletic activities. They do not necessarily make up the iron loss of menstruation at the time that the need increases. Some of the early periods can be irregular and very heavy too compounding the problem.
– Athletic female teens are increasingly engaging in strength training as part of their sports practice, which is excellent news for the overall health, bone health, and injury resilience. The main protein founded muscle is called myoglobin, which requires a lot of heme iron to manufacture. This is the same heme iron that incorporated into the red blood cell hemoglobin. Practically this means that strength training diverts some of the heme iron resources into muscles and away from red blood cell production, increasing the risk of anemia. This phenomenon has sometimes been referred to as the myoglobin shunt.
– The complex landscape of teenage eating habits, tied into body image, food preferences, and some desire to pursue more vegetarian diets, can often lead to very low content and bioavailability of iron and supporting minerals in the diet.
Assessing an athletic female teenager for the potential of suboptimal iron reserves as a migraine trigger is not as straightforward as you would think. The body is very good at compensating for low iron and maintaining apparently normal routine lab values for a very long time. In order to really assess the iron status, a patient will need a CBC, iron panel including ferritin, which is often the first value to drop before seeing any changes in the red blood cell count. My rule of thumb with our young athletic females is to see a ferritin in the 50 range, to give the margin for fluctuations during the menstrual cycle. Be aware that technically the range of what's considered "normal" ferritin on many of our labs is as low as 10, which is clearly not sufficient for most people much less someone involved in high-intensity athletics.
Restoring normal iron and hemoglobin reserves is also not a straightforward as you would think. Common iron supplements tend to be very irritating to the G.I., resulting in constipation, poor compliance, and not necessarily improving iron levels. My recommendation is to combine more easily absorbable forms of iron with cofactors of copper and zinc, and take them and minimum of twice a day, in smaller doses, and ideally three times a day for the first 30 days until the patient starts feeling better. This obviously should be in addition to changing dietary pattern to have more bioavailable forms of iron for a couple meals a day. In addition, I want to make sure that the athletes is having a pre-workout electrolyte and creatine bolus, and that they have had adequate caloric intake including some healthy form of carbohydrate no more than two hours before an intense exercise session. This will help support sustain energy production for their body and their brain during exercise. Ferritin should also be monitored at six weeks, and 12 weeks, to make sure you adjust the supplement dose into a healthy non-toxic range over time.