It's a question that comes up frequently and I realized recently that I don't have a good written resource material to direct patients to and I find myself repeating the same thing over and over in the middle of a busy day. Unlike some of my colleagues, who tend to downplay their value in an overall treatment plan, I feel that topical's can have huge benefits to direct therapeutic activity to a local local area, and can overall minimize the patient's need for more toxic oral medications.
Understand that this is a generic list, and that you will probably need to figure out with your own individual healthcare provider which 1 of these may be the best, and understand that you may need different topical treatments at different times. Also understand that while mostly safe, a few of them do have some potential contraindication related to other medications and comorbidities that you should be aware of.
Topical treatments full in different broad categories matching their mode of action: counter irritant, vasodilators, anti-inflammatory, analgesics, and some of them crossover into more than one category.
COUNTER IRRITANTS: those agents tend to create a local receptor response that competes with pain receptors, thus tricking the body in perceiving sensation rather than pain. Menthol is probably the most common one. It's found as a base in the majority of topical treatments. It's usually quite safe, short acting and reversible. There's a huge variety of products available, and ultimately it boils down to preferring water-based versus oil-based, and how much of an overlying sent or not you want to have.
VASODILATORS: those agents tend to increase local blood flow by increasing vasodilation of smaller blood vessels. The main benefit is to improve circulation to a particular area, especially in the periphery of the body. The main ingredient is capsaicin, derived from hot peppers. On the tail end of the activity, they tend to have a mild analgesic effects. The benefits are to improve blood flow to deliver soft tissue repair nutrients, especially oxygen, in areas that are having a hard time healing or are somewhat avascular because of previous trauma or general health issue with blood circulation. You have to be quite careful with them, since they can create great irritation to the skin, and they are more medical contraindications to using them, especially with peripheral vascular disease and diabetes. It comes in different potencies, and you also have to be extremely careful not to rub your eyes after applying them.
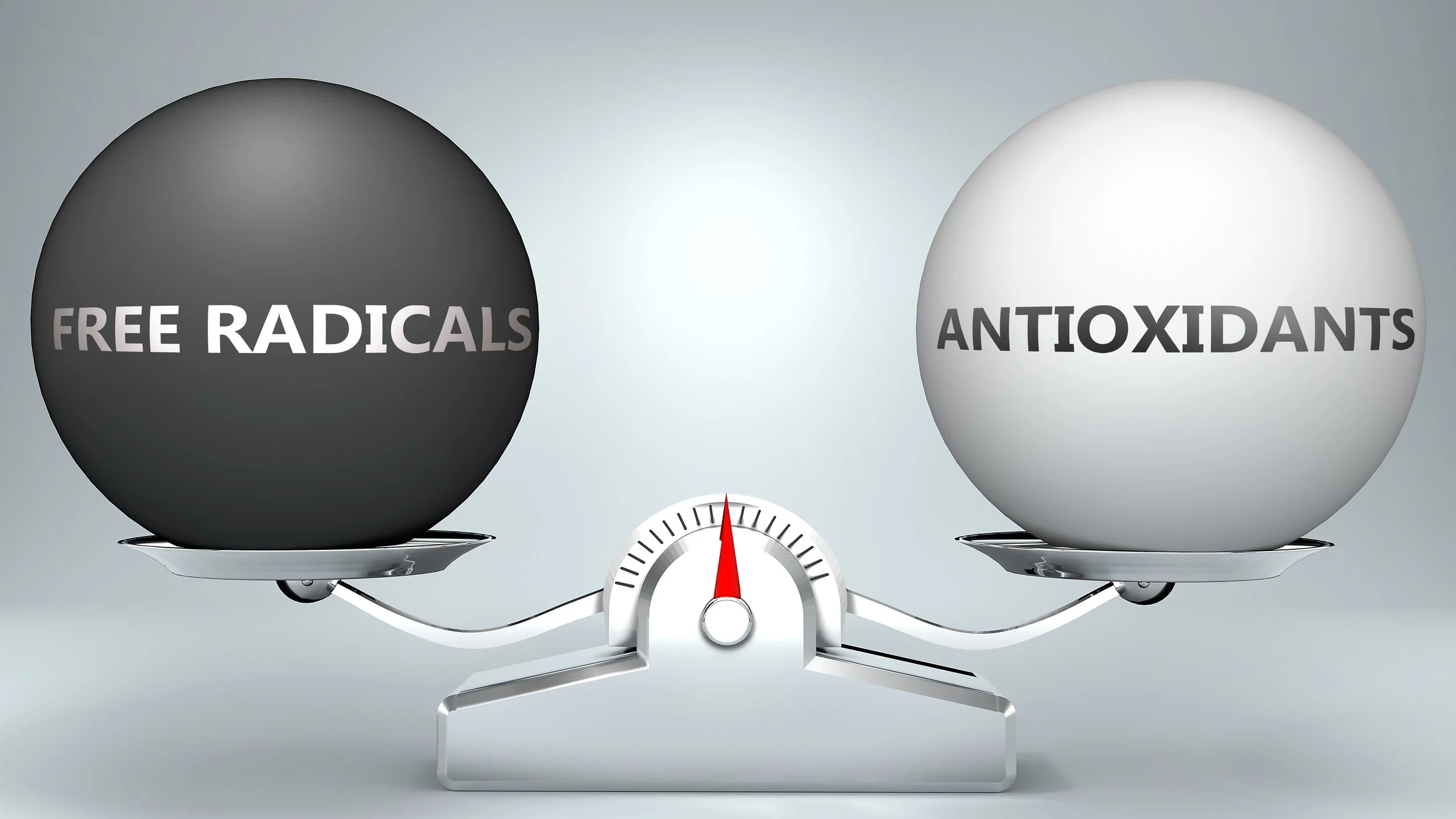
ANTI-INFLAMMATORIES: it's a relatively broad category, with many agents having a secondary anti-inflammatory effect in addition to another primary effect. The effect pathways of information in peripheral tissue. This includes both pharmacological over-the-counter substances as well as naturally occurring substances.
- salicylate and dicofenac are topical versions of pharmacological oral equivalents, which are available over-the-counter. (Aspercream or generic equivalent is the most common version). They are quite effective, have a moderate acting range, but have to be used very carefully especially if it's used consistently in the long term because it does eventually reach your bloodstream. I think there is definitely a time and a place for short-term use during acute trauma recovery, to minimize the need for oral pain medication. There are some definite contraindications, so best to check with your provider before using.
-Essential oils like frankincense: should be used in small amounts in a carrier oil because of their potency, but can be a very nice long-term alternative because in smaller doses they really quite safe.
- Arnica: increasing in popularity in the US, I grew up with Arnica as a mainstay in our pharmacy box. It's a little bit of an atypical anti-inflammatory, which is used mostly for acute trauma and contusions. It has virtually no side effects so that one is safe for just about everyone to try.
- CBD: an oil-based extract from the hemp plant, CBD alone has no psychotropic effect and is relatively easy to use in the long term quite safely. I find that CBD takes a little bit to kick in, and I think it's best used for long-term management of chronic joint or soft tissue inflammation rather than as an acute aid.
- MSM: a sulfur based compound, it has a great safety profile when used topically. It has a mild anti-inflammatory effect, but is primarily used to support chronically injured collagen, such as osteoarthritis of joints, and chronic ligamentous or tendon injuries.
ANALGESICS: it's a little bit of a difficult category to pain, since analgesics means pain reducer. The mechanism of pain can vary in different patients, so all of the above can act as analgesics in a particular patient. However technically only very few compounds are considered true analgesics and they are relatively uncommon. The most commonly available over-the-counter is a pharmacological compound called lidocaine usually applied in transdermal patches. Lidocaine is powerful, short to moderate acting, but it has a fair amount of side effects and many medications adverse interactions for a lot of people so I would use that one was a lot of caution and with the green light of your provider. There are very few nonpharmacological true analgesics, such as California Poppy.
This is not an exhaustive list, with several other less commonly used compounds such as homeopathic's, and many bundled products. But this should at least be enough of a background for patients to start asking the right questions to select the right topical for their personal use.