It’s another 1 of those questions I field almost every day, and for which I finally decided to write a reference blog to direct patients to.
The short answer is yes, and the devil is in the complicated details. Patients will often ask that question when they're presenting with a type of shoulder pain that feels very "nerve like", and have been told that there is no pinched nerve in the cervical spine to account for the pain. It's important to note that a large proportion of shoulder pain can indeed be referred nerve pinching pain from the cervical spine.
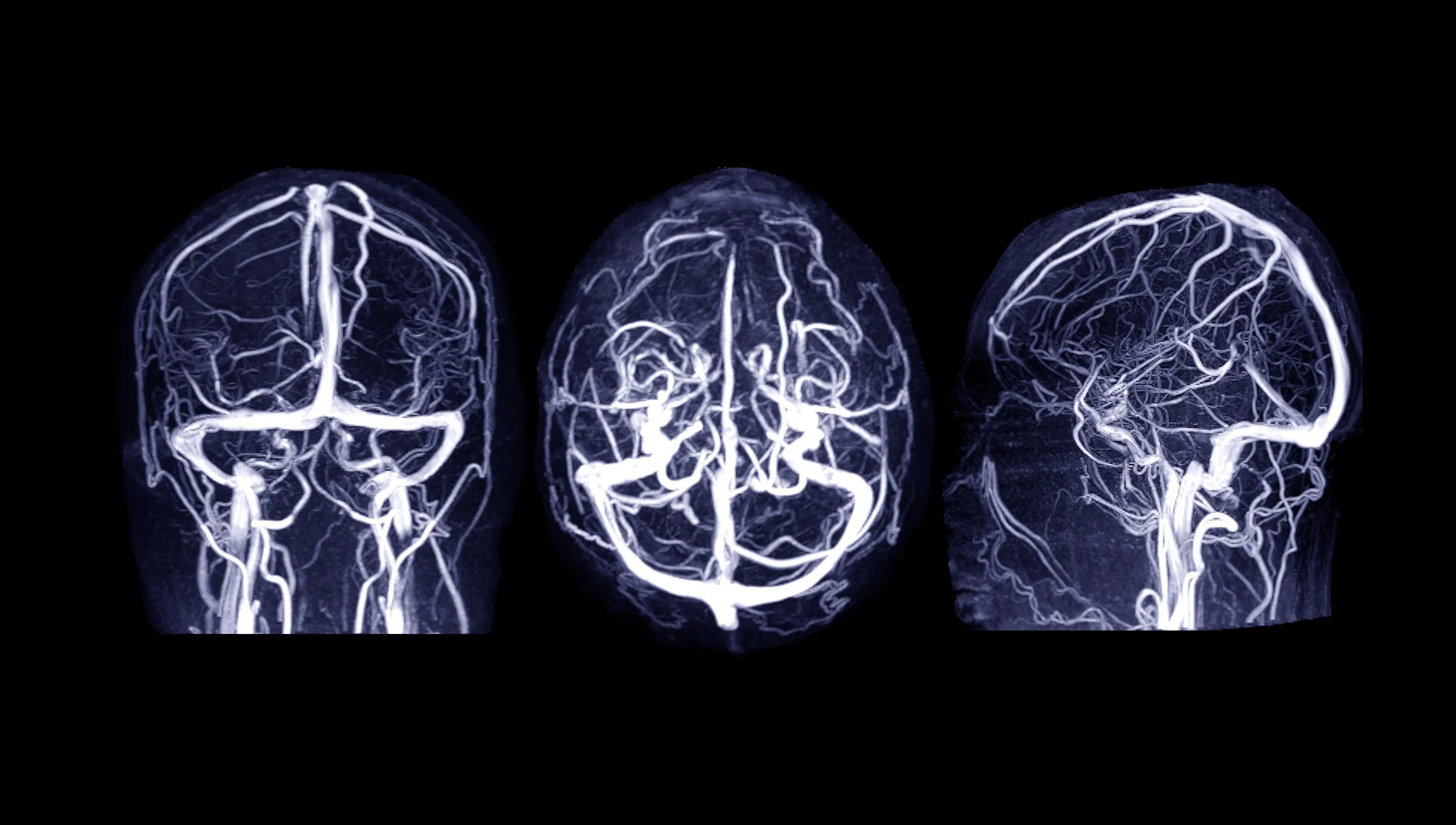
If you want to get clinical, and if you consider the shoulder a broad area from the lower neck into the upper arm, from the clavicle to the shoulder blade, the number of peripheral nerves you can entrap is surprisingly high, but in this blog entry I wanted to focus on four neurological structures that are subject to impingement from functional shoulder disorders (misalignment, trauma, muscular imbalances especially): the brachial plexus, the suprascapular nerve, the long thoracic nerve, and the axillary nerve. As you can see from the various images, they are distributed in various parts of the shoulder girdle close to neuromusculoskeletal structures such as the shoulder joint, the clavicle, and various deep muscles of the shoulder. Of these 4 structures, the brachial plexus receives the lion share of the peripheral shoulder entrapment syndromes, because of the length of its path from the lower cervical spine into the upper arm, and the number of structures it has to traverse. It also gives rises to several of the secondary peripheral nerves. Incidentally almost all of the peripheral nerves travel alongside with correlating vascular structures, meaning that peripheral nerve entrapment syndromes also are often jointly vascular entrapment syndrome (with symptoms associated with decreased blood flow to an area). Developing shoulder entrapment syndrome can be both acute and chronic, often the result of long-standing postural shifting of the shoulder, as well as one trauma or acute sprains. Ultimately treating the underlying mechanism of nerve entrapment is the best way to address them.