I was joking with a colleague that there are some "sexy muscles" that seem to be popular from time to time, but the one I'm about to blog about is definitely not in that category. Which is unfortunate because it can be an absolute source of misery.
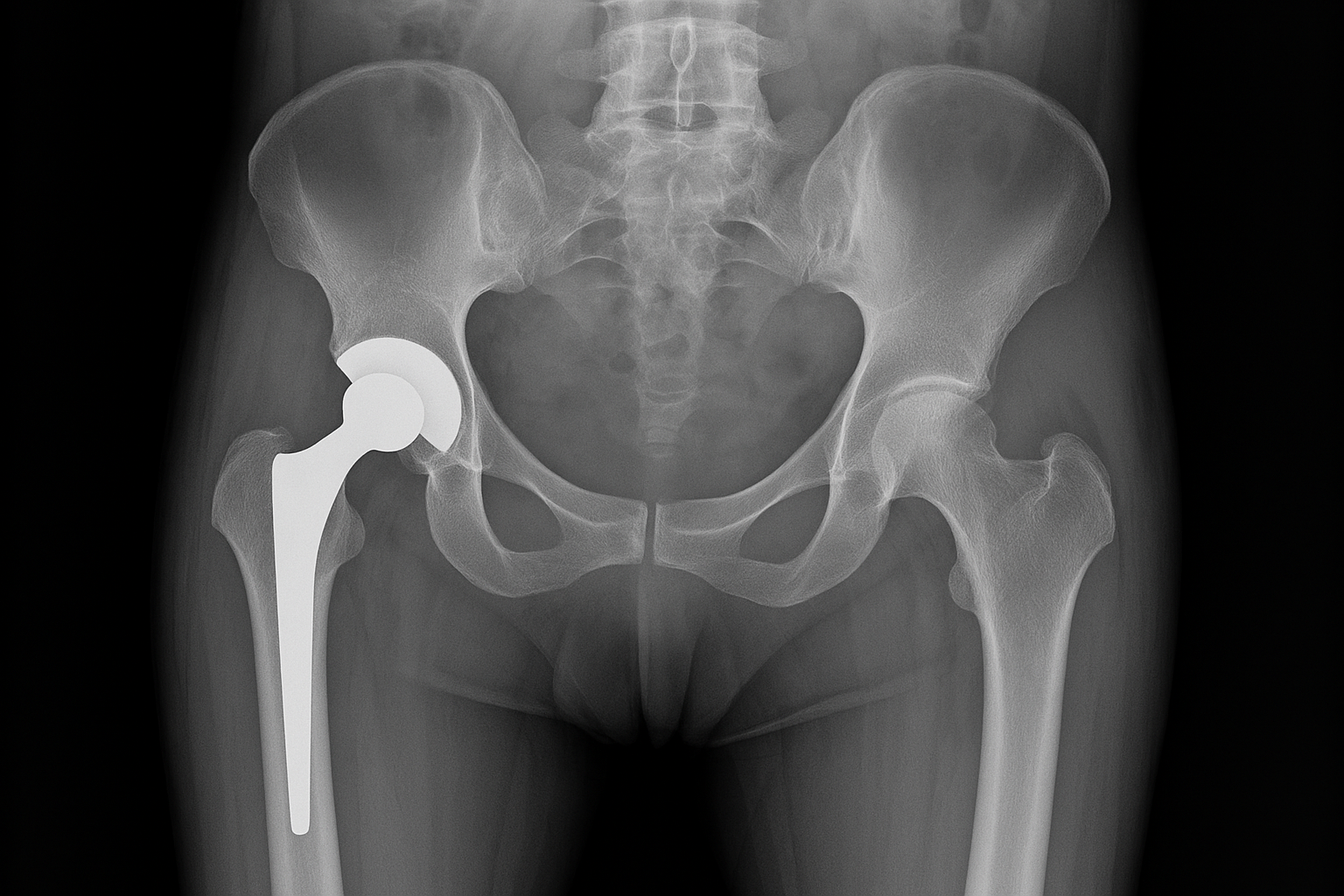
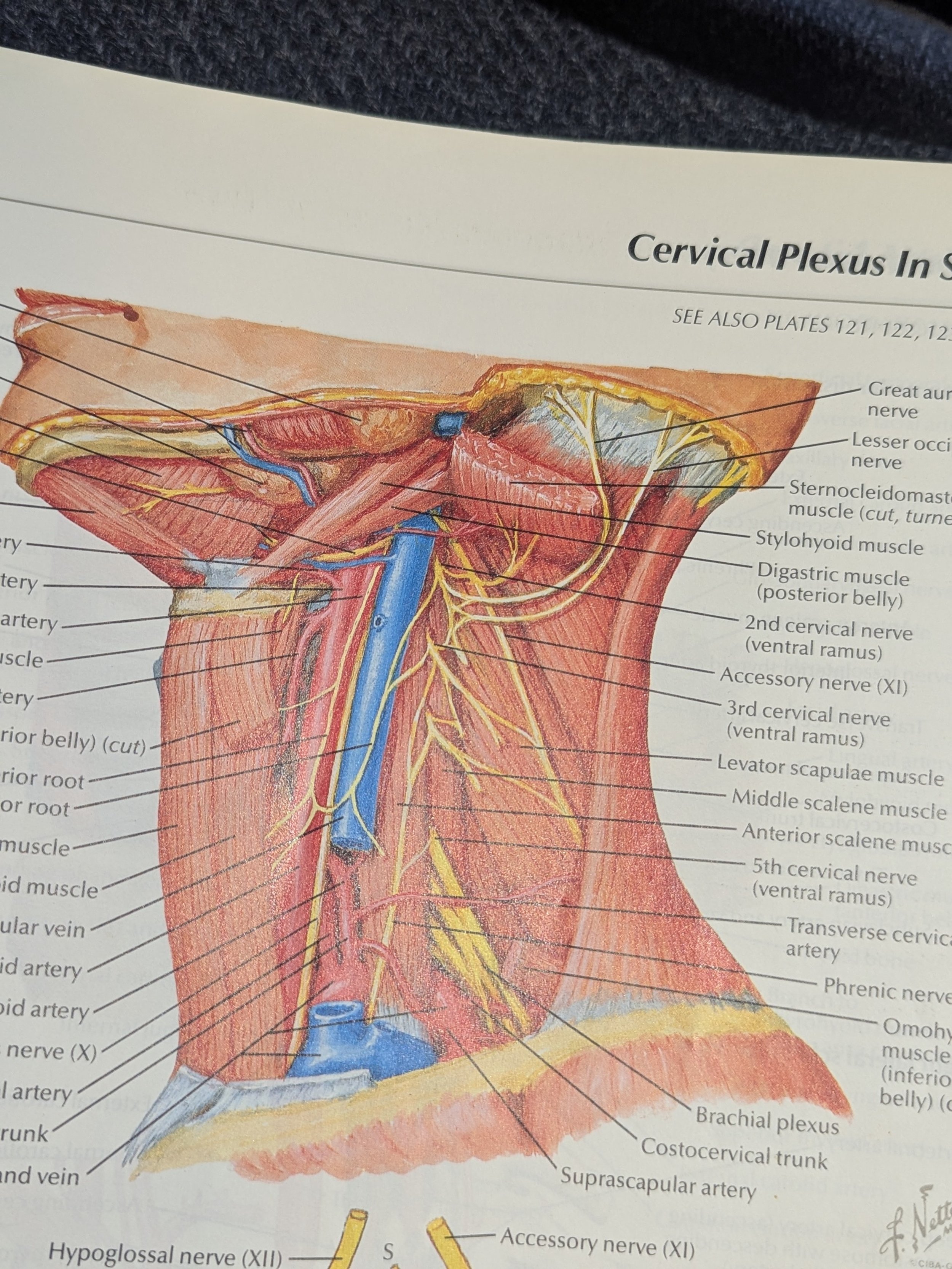
The obturator externus, later referred to as OE is a muscle that is deep in the groin, connecting the anterior inferior part of the pubis to the inside of the upper femur. It's involved in a combination of adduction stability of the leg (and thus can be injured in sharp abduction sprains), with lesser degrees of rotation and flexion. It's not easy to palpate unless you know exactly how to locate certain origin and attachment landmarks, and it connects different parts of our anatomy that make it involved in activities of the leg, trunk and pelvic floor at the same time. The pain pattern usually involves the inside upper thigh, groin, but can also radiate to the perineum and lower abdomen. Mechanism of injury include leg abduction and flexion sprain, slip and trip injuries, weightlifting injuries, and more repetitive type overload injuries such as anterior position of pregnancy and long-distance running.
The reason that the OE is worth talking about is that it can be a source of continued pain even when other parts of an injury have resolved. I have encountered that in many cases where we successfully treated and rehabed sacroiliac and upper thigh injuries for example, but the patient continued to have some very pinpoint groin pain that continue to prevent them from resuming their previous activities. It's often an area that the patients are hesitant to talk about because it will radiate into the genital and pelvic floor area, as well as deep in the inside of the thigh, both areas the patients don't necessarily like to have examined. And an area that many health care providers don’t like to dig in.
Treating and resolving an OE painful syndrome can be a game changer for patient. I'm grateful for my ART training 15 years ago to give me the confidence to properly locate the muscle and perform the appropriate myofascial release on it. The OE responds surprisingly quickly to therapy, usually clearing up within 2 or 3 treatments. It's a little tricky to stretch at home unless you know how to combine the 3 motions to isolate it. I have found my best results with the modified unilateral elevated cobbler with some butterfly flexion.