I had a discussion last week with one of our teens involved in athletics, followed 15 minutes later by a similar discussion with a patient in his 70s, struggling to improved metabolic syndrome and stabilizing old athletic injuries. The common thread was the importance of high quality balanced sufficient protein intake in achieving their goals (respectively mitigating chronic returning injuries and managing diabetes). Looking at my weekly research digest with this particular article at the top come up I knew the universe was telling me to put up a blog about it.
The importance of protein intake comes and goes in the integrated and wellness space. That's unfortunate because it should never leave the discussion .It's just one of those subjects that's not sexy enough to make headlines and money on a consistent basis so it gets cycled through when it's convenient.
For the sake of keeping this blog entry at one page rather than 20, I just want to highlight a few key points in regards to protein intake:
· The total intake for optimal health and maintenance of lean muscle mass and soft tissue repair is about half a gram per pound of body weight, as a very crude measurement .Which means that for an average adult it's going to be close to 80 grams a day, much less than what most people are getting. It can even go higher in certain needs such as increased physical activity, recovery from illness injury surgeries or other trauma.
· Quality of the protein is also crucial. It is defined as the diversity and percentage of essential amino acids, defined as those that cannot be manufactured by your body. In that regard animal protein has a much better profile since it belongs to animals, rather than plant based protein which are meant to build up plants. This statement will often cause quite a stir among people who are advocating a plant based diet. But understand that recognizing the importance of the quality of animal protein does not necessarily mean that it makes up the exclusive protein source in your diet. It means that it needs to be present in meaningful amount to provide the needed amino acid mix, but that plant based protein that are part of the plant part of your diet is also beneficial. If you look strictly at the data and the research it's very difficult to get optimal protein intake and amino acid balance from a plant diet alone without resorting to some very fractionated supplementation. My ballpark figure is to get at least half of your protein from animal sources. Ideally flesh based protein should be nose to tail and incorporate not just muscle meat but organs and connective tissues, As well as sea and land animals.
· Incorporating animal protein can be done with respect to environmental and animal welfare concerns. In that regard we are very fortunate in our zip code to have access to ethically raised and properly fed sources of animal protein.
· Incorporating optimal amounts of diverse protein in your diet will also have a beneficial effect for weight management. Our brains are engineered to continue eating until we have extracted enough essential amino acids from our food. Thus our brains are less likely to continue hungering for calories if the total amount of essential amino acids has been met. Conversely, if the amino acid density is low, your brain is going to signal you to continue eating more food, thus calories until you reach that sufficiency point.
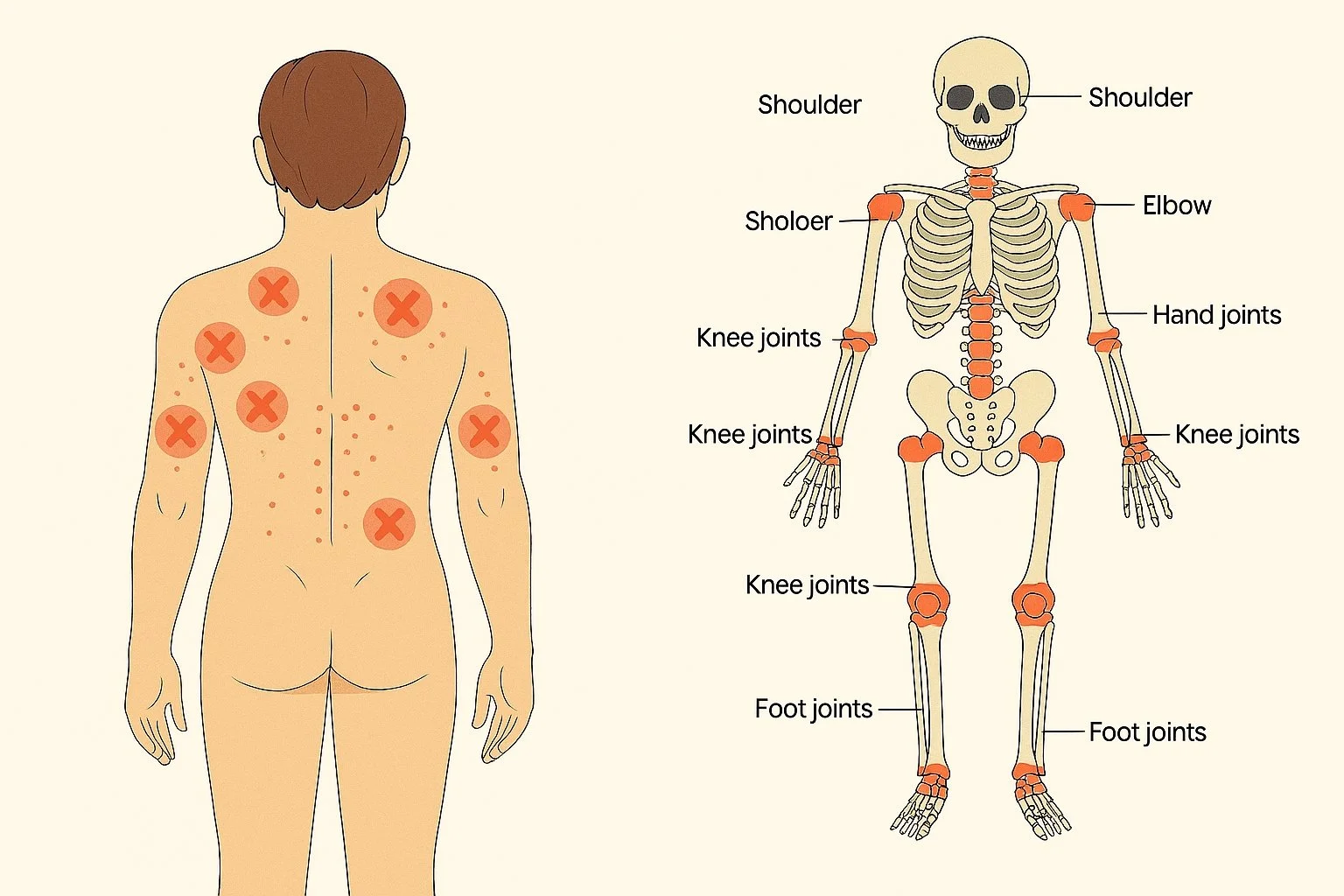
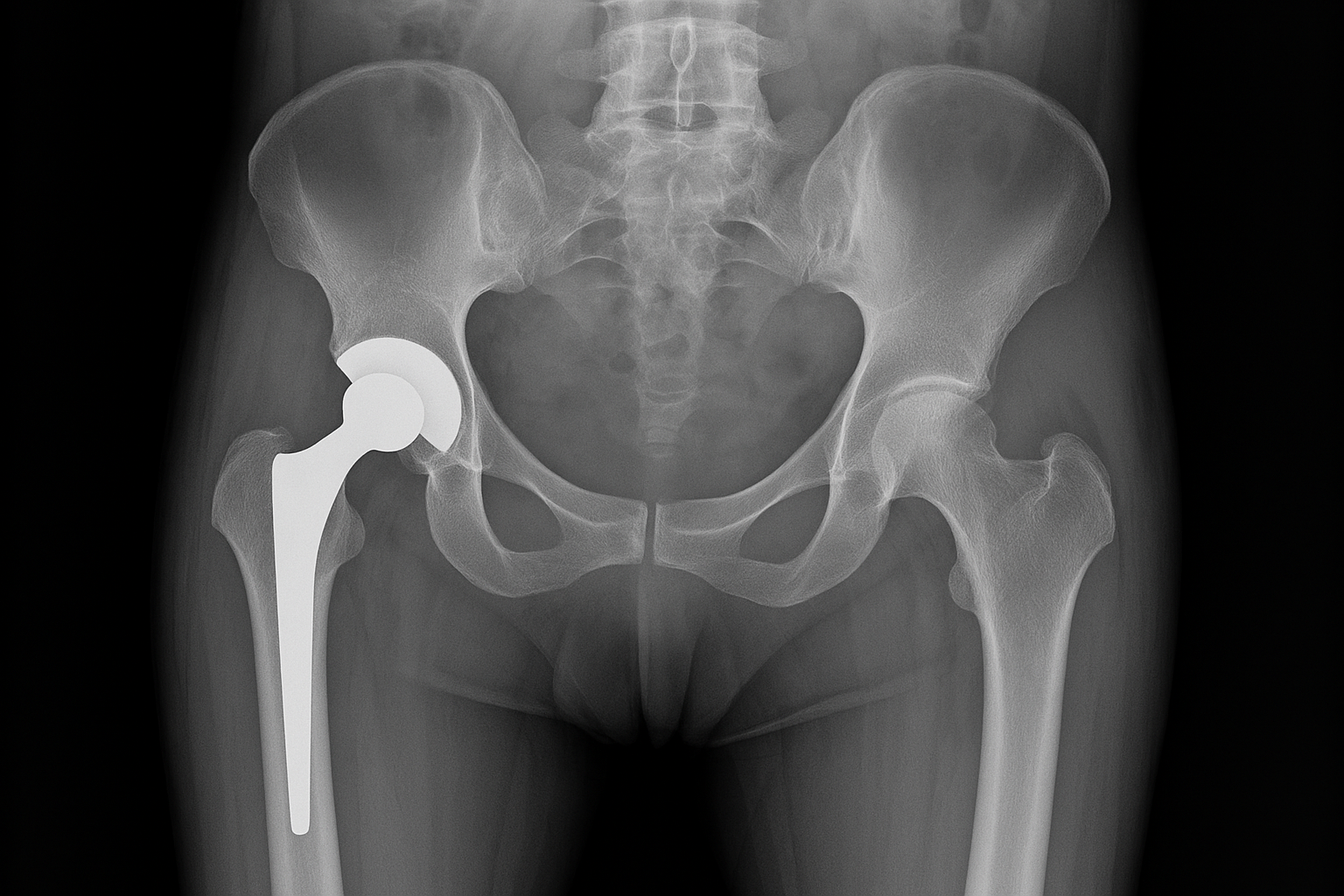
· Protein sufficiency is important at every age but in the instances of the two patients I saw back-to-back, for very different reasons. Our athletic teen kept having recurrent tendon and muscle injuries because she was grossly deficient in adequate protein for normal repair during a high intensity season with daily 2 hour practice. Our 70 year old with metabolic syndrome was seeing low results from his strength training program and poor control of diabetes because he was not able to leverage his exercise into the deposition of lean muscle mass due to suboptimal protein intake. Numerous studies have shown that adequate protein intake becomes more crucial as you age, since our body is less efficient at extracting amino acids and depositing them for the same amount of protein you eat 10 years earlier.
· The question over protein powder continues to come up as part of the protein sufficiency discussion period my first recommendation is to always get as much of your protein intake from Whole Foods, and supplement no more than 25% maximum with protein extract. This would mean practically that one serving of a protein powder concentrate of about 20 grams per day is OK at times, but should not be the default to meet your protein needs. It is however a very smart move during certain times when getting the right amount of protein may be difficult, such as some of our patients dealing with aggressive treatment with chemotherapy, recovering from oral or GI surgery for example. Protein powders come in very different qualities, and maybe beyond the scope of this blog to discuss. As a general rule you should not use plant based protein for large amounts of protein supplementation due to amino acid balance, and as long as you have tolerance for dairy, whey protein, egg protein, and sometimes hydrolyzed meat proteins may be a better option. However remember that certain simple dietary hacks such as a can of tuna, a cheese stick, a couple of boiled eggs can give you a pretty good 10 to 20 gram boost with not a lot of calories.